Revenue Cycle Management
Introduction to Revenue Cycle Management
Eligibility
Medical Insurance Authorization
Revenue Reconciliation
Denials
Revenue Recovery
Quiz
Resubmission 2
RESUBMISSION
Resubmission is a process of submitting a previously denied claim in accordance to the Electronic Visit Verification [EVV] guidelines.
FAKE BILLING
This is a technique used in the resubmission process to help ensure a successful resubmission. It involves resubmitting a claim with certain deliberate errors with the intention of getting a different denial reason other than the initial. This will help facilitate resubmission. Once the fake billing is denied, the claim number is used for proper resubmission.
FAKE BILLING PROCESS
- Sign in to the United Healthcare [UHC] and TMHP Portal simultaneously
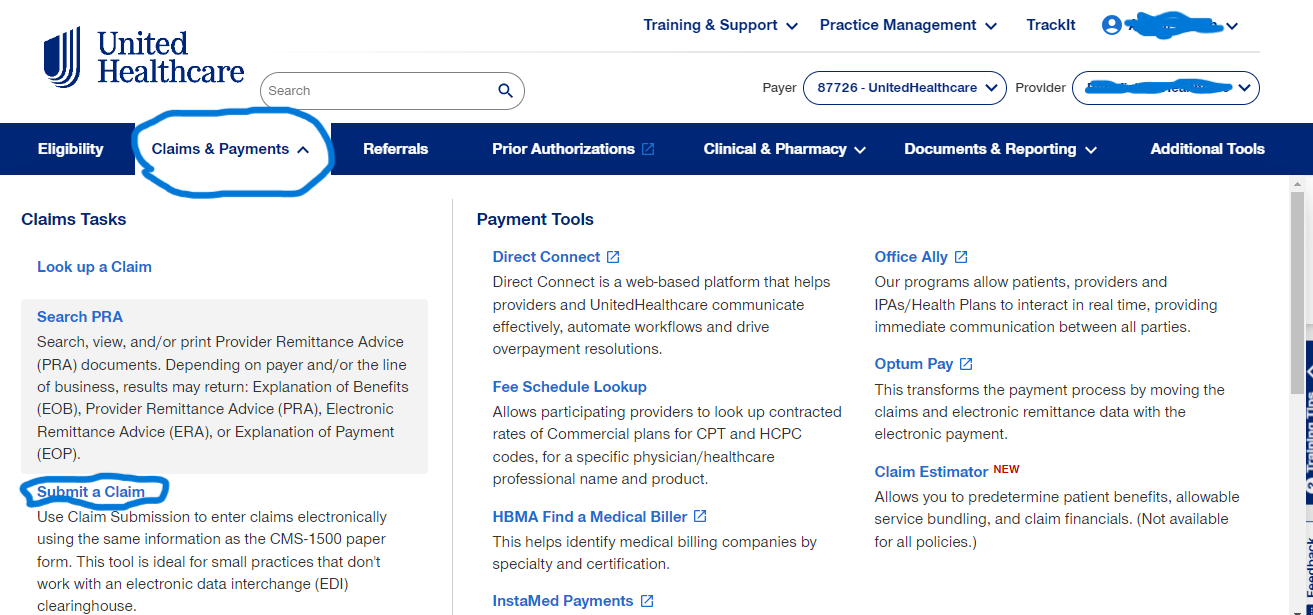
- At the top Ribbon, Click on Claims and Payment
- Click on Submit A Claim
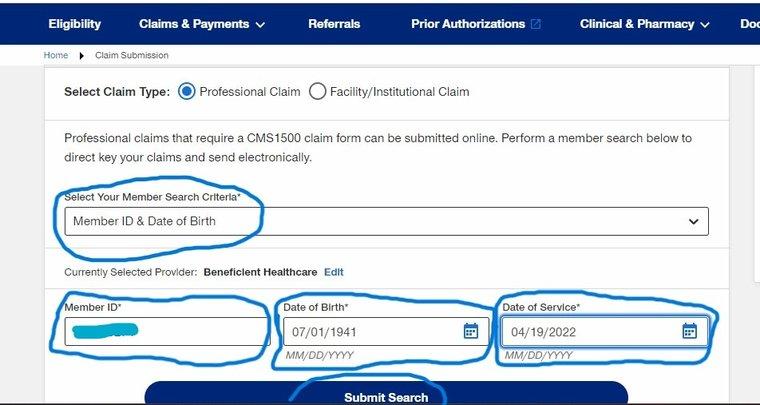
- On Select on Member Criteria Select Member ID and Date Of Birth and fill the Member ID, Date of Birth and Date of Service
- Click on Submit search
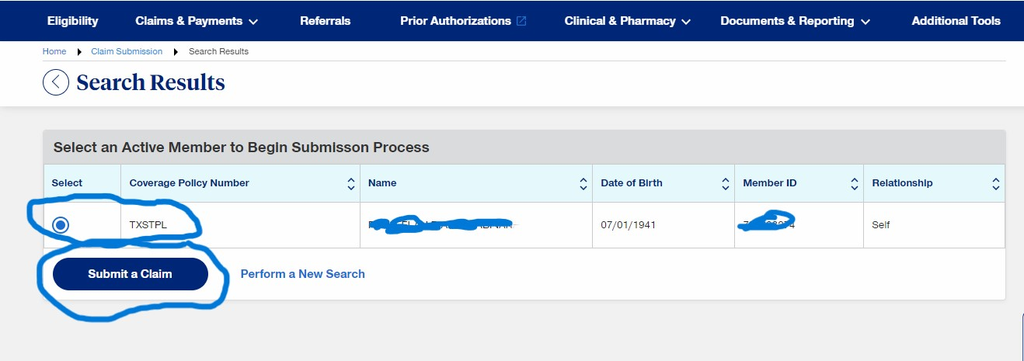
- On Select an active member to begin Submission process select TXSTPL and click Submit a claim
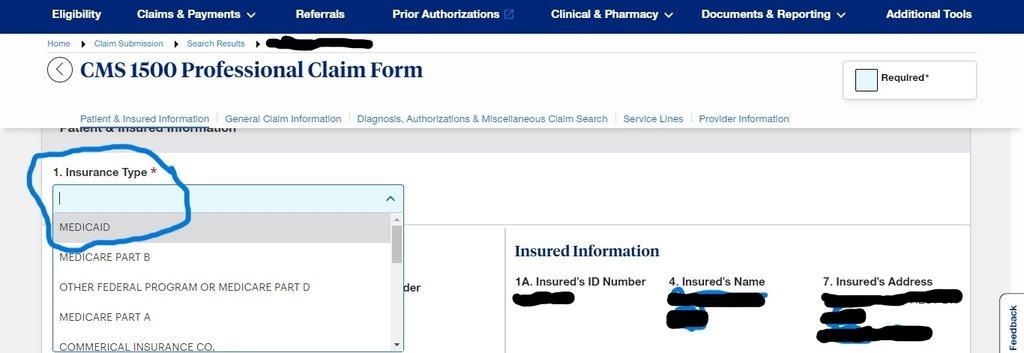
- On Insurance Type, Select Medicaid and scroll down
- Patient information and insured Information is Auto Populated then stroll down
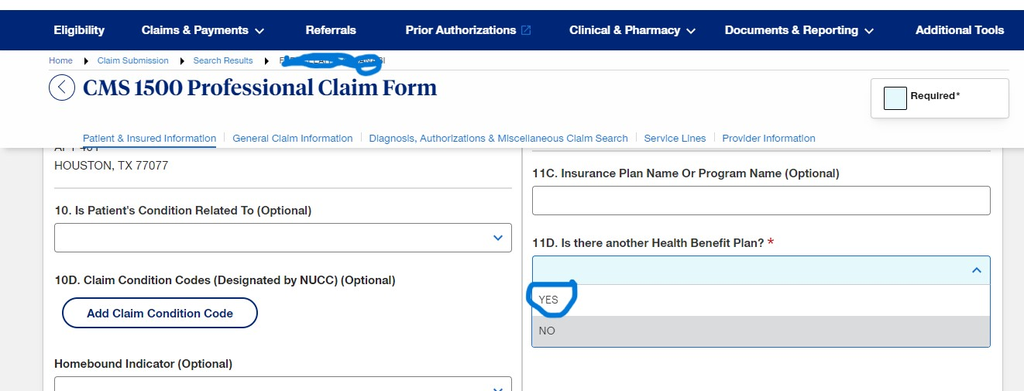
- On: Is there another Health Benefit Plain Select No then scroll down
- General claim information is Auto Populated
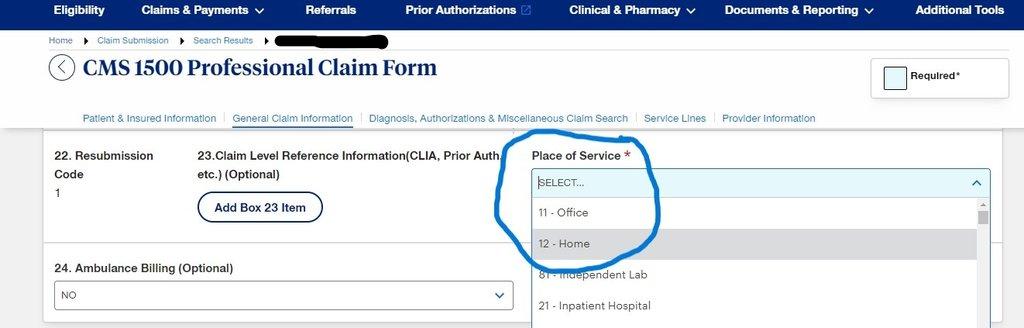
- On Place of service Select Home
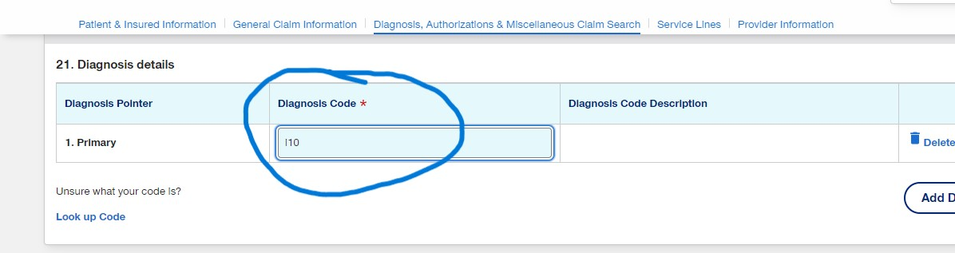
- For Diagnosis Details, fill in the diagnosis code scroll down
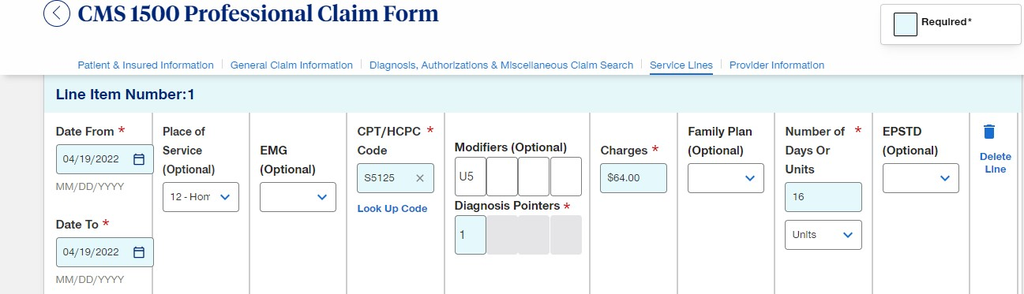
- On Line item number 1, Fill in the Date From [use a more recent fake date], CPT/HCPC Code, Modifiers option, Diagnosis Pointer, Number of days or Units with the appropriate denied claim information as seen below and scroll
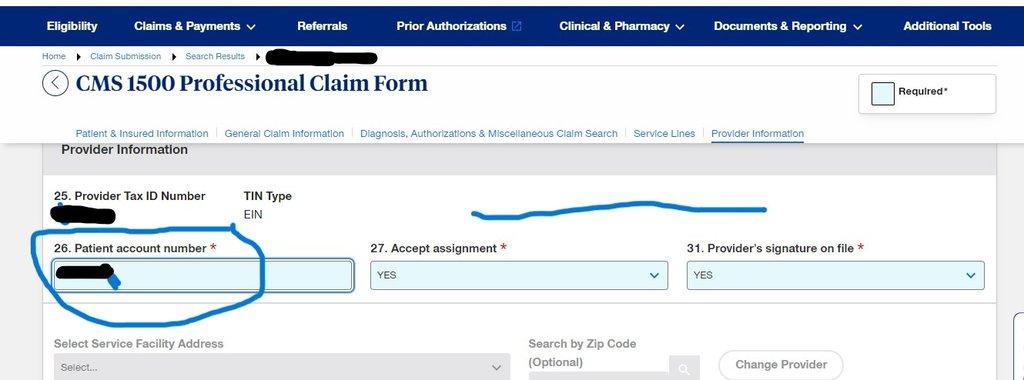
- On the Provider Information, fill in only Patient account number other information is auto populated then scroll down
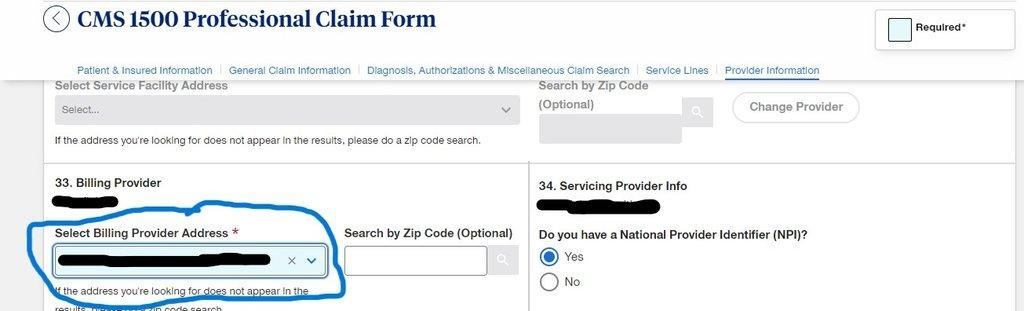
- On Select Billing provider address, select 202 Industrial BLVD STE 204 Sugar Land then scroll down
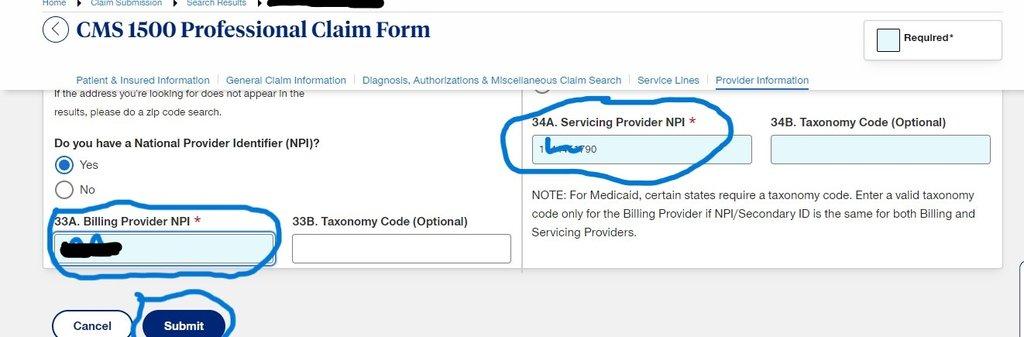
- On Serving provider NPI and Billing provider NPI, fill in the same NPI Number and click Submit.
RESUBMISSION PROCESS
- Sign in to the United Healthcare [UHC] and TMHP Portal simultaneously
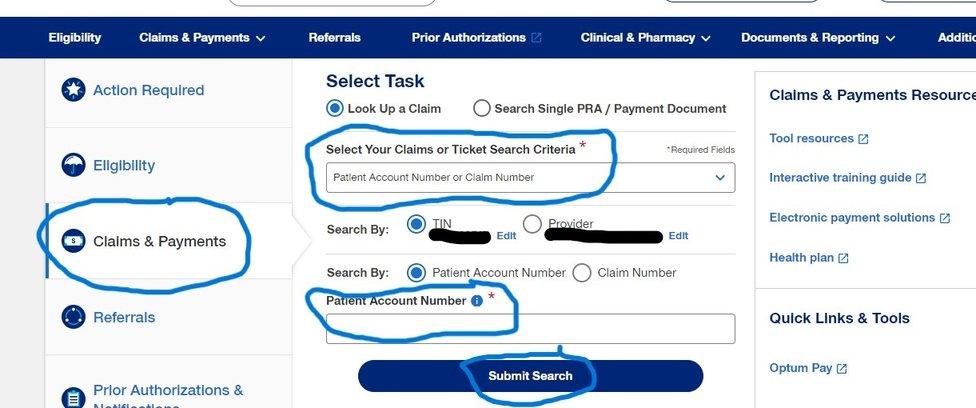
- Click on Claims And Payment
- On Select Your Claims Or Ticket Search Criteria, Select Patient Account Number Or Claim Number, and on Patient Account Number, Fill In the Member ID, then Click On Submit Search
- On Claims Result, Trace the Fake billed claim[using the fake date] and click on the claim number to get into claim.
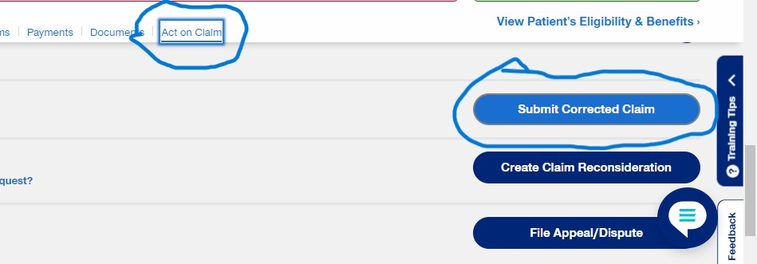
- Click on Act on Claim then click on Submit corrected Claim
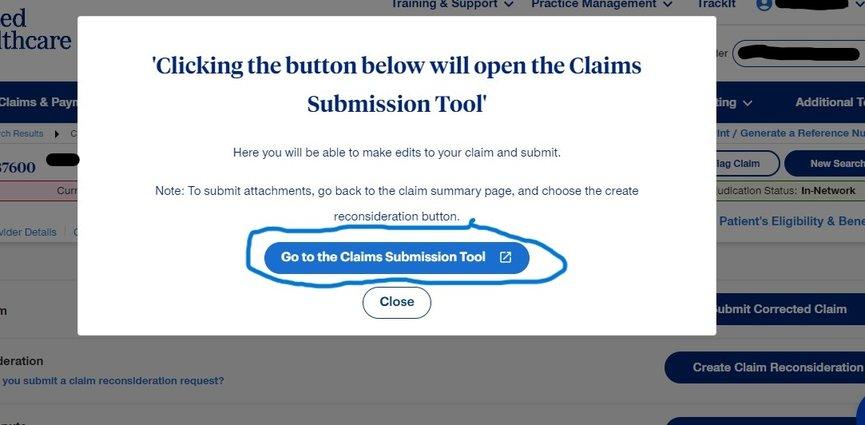
- Click on Go to the Submission tool.
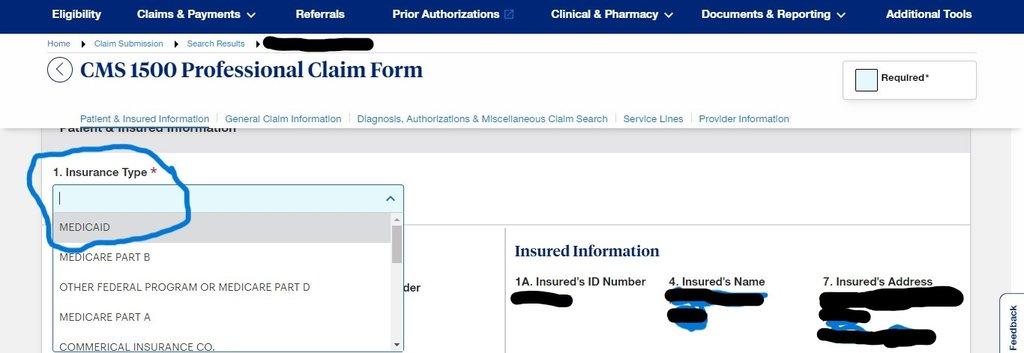
- On Patient & Insured information, select MEDICAID for insurance type while other info is auto populated then scroll down to Line item number
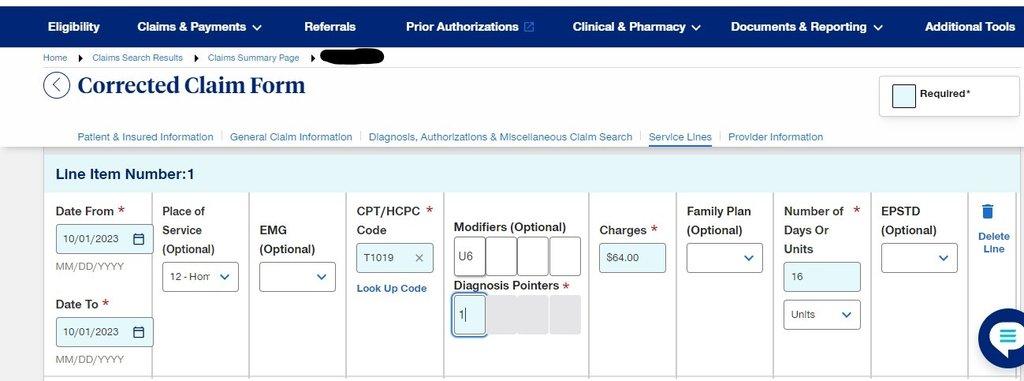
- On Line item number, use the TMHP Portal to fill in all necessary details. [inline with the Electronic Visit Verification EVV]
- Click on Add Row to add more rolls and repeat the same process from the previous.
- On Provider Information, fill in the NPI number for Servicing provider NPI and Billing Provider NPI then submit.

Have a doubt?
Login