Revenue Cycle Management
Introduction to Revenue Cycle Management
Eligibility
Medical Insurance Authorization
Revenue Reconciliation
Denials
Revenue Recovery
Quiz
Eligibility
Eligibility Checks: A walk through
Eligibility checks should be carried out regularl, preferably in a structured manner with predefined dates. One way could be to carry out checks 3 time a month, on the 1st day, the 15th day and the last day of every Month.
Here are two different examples of how eligibility checks can be carried out
1st Way
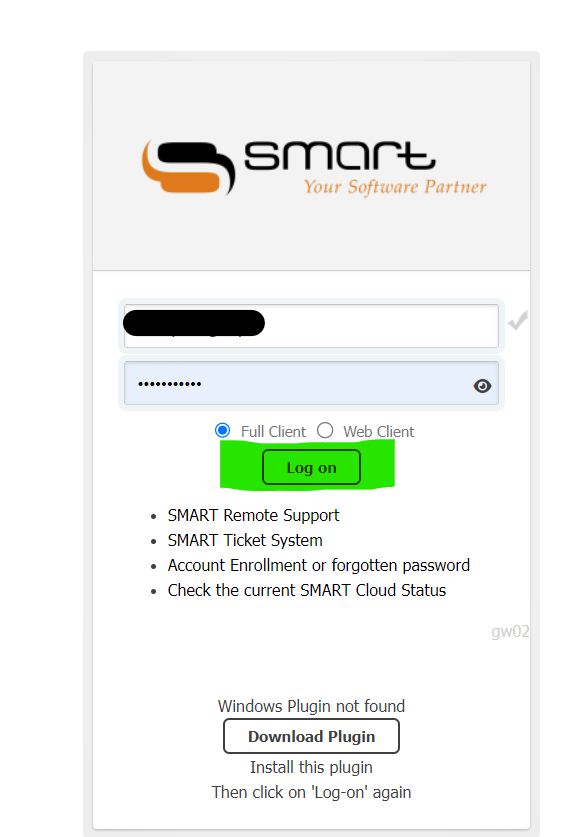
- Log on to the Smart App
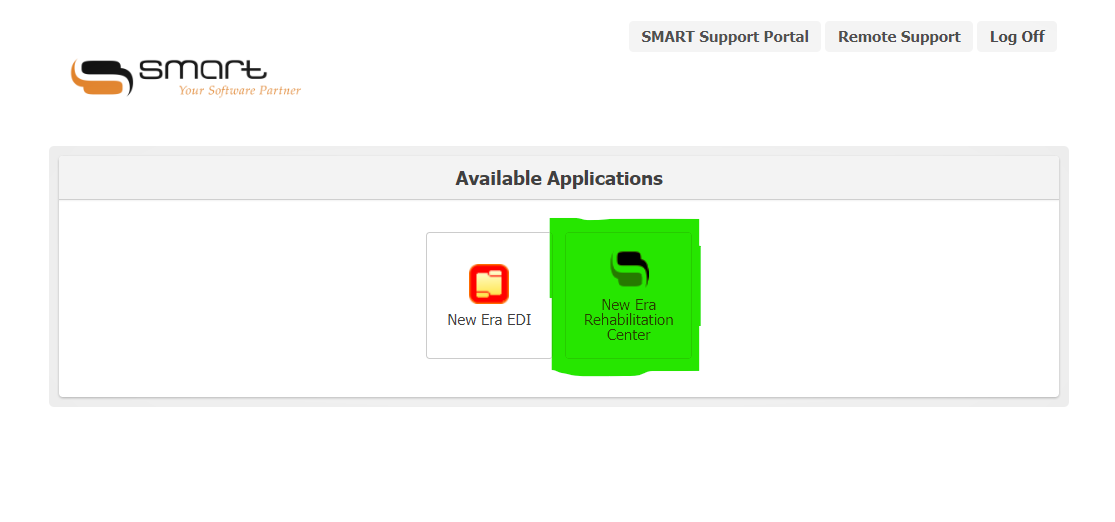
- Click on New Era Rehabilitation Center icon
- Click on the Print icon
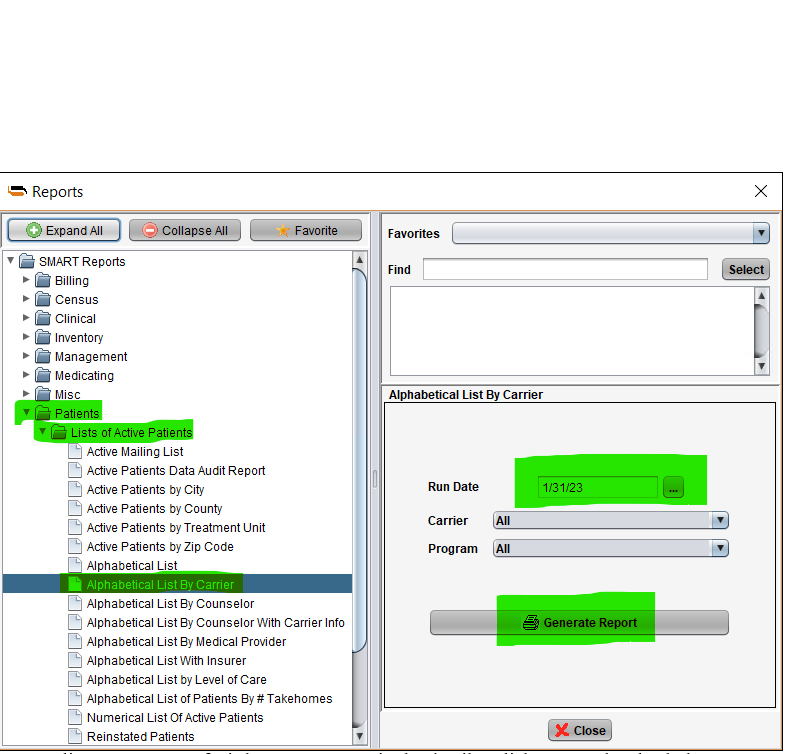
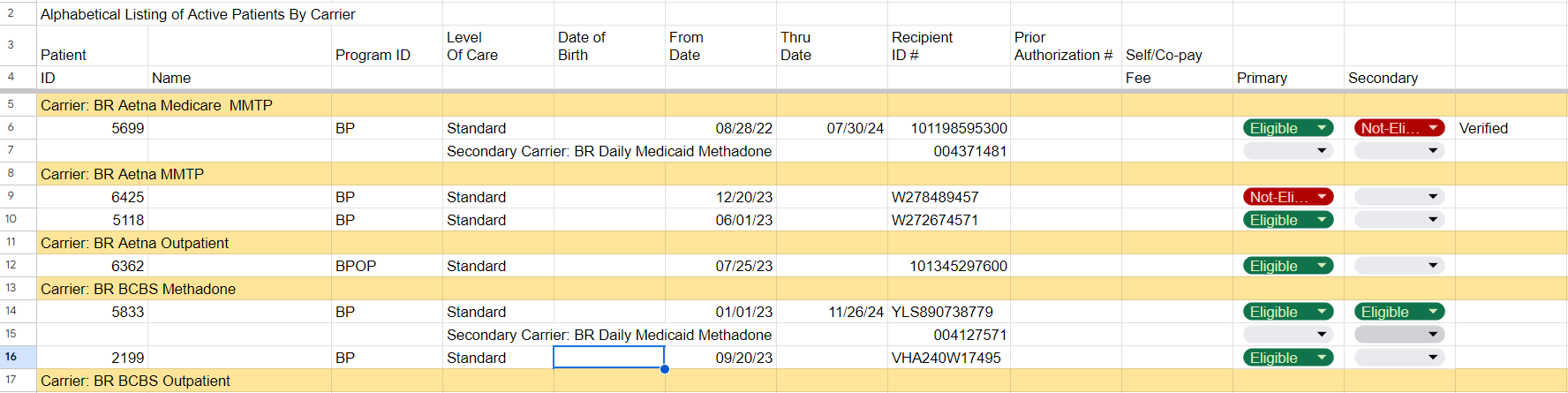
- Click on Patient ----- List of Active Patient ---- Alphabetical list by carrier (You’d see a full list)
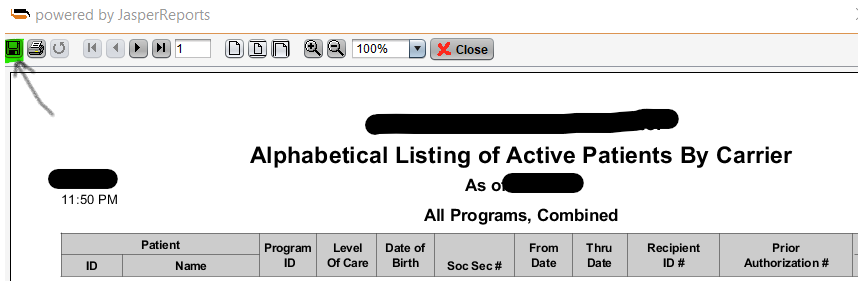
- Click on ‘Generate Report’ (The report pops up)
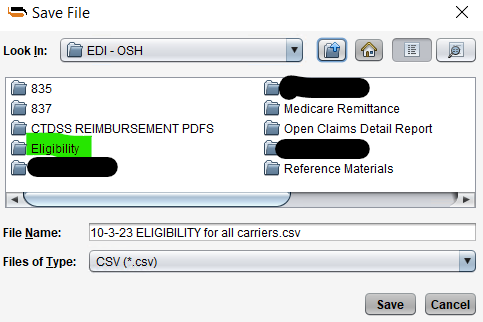
- Click on Save --- Export --- New Era--- EDI File --- Change the file type from pdf to csv --- Save in the Eligibility Folder (date first, Carrier). Close the page
- Open New Era EDI --- Look for Eligibility
- Copy the file & paste it on your desktop.
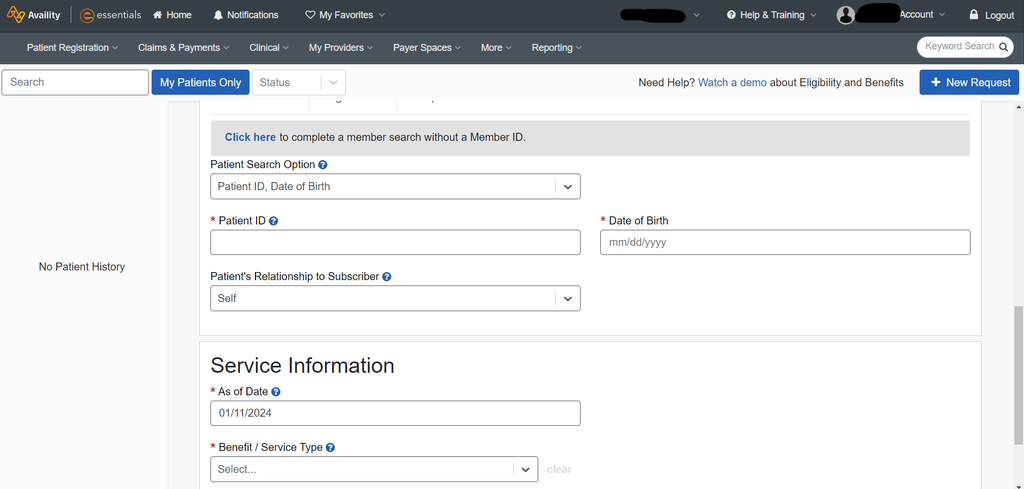
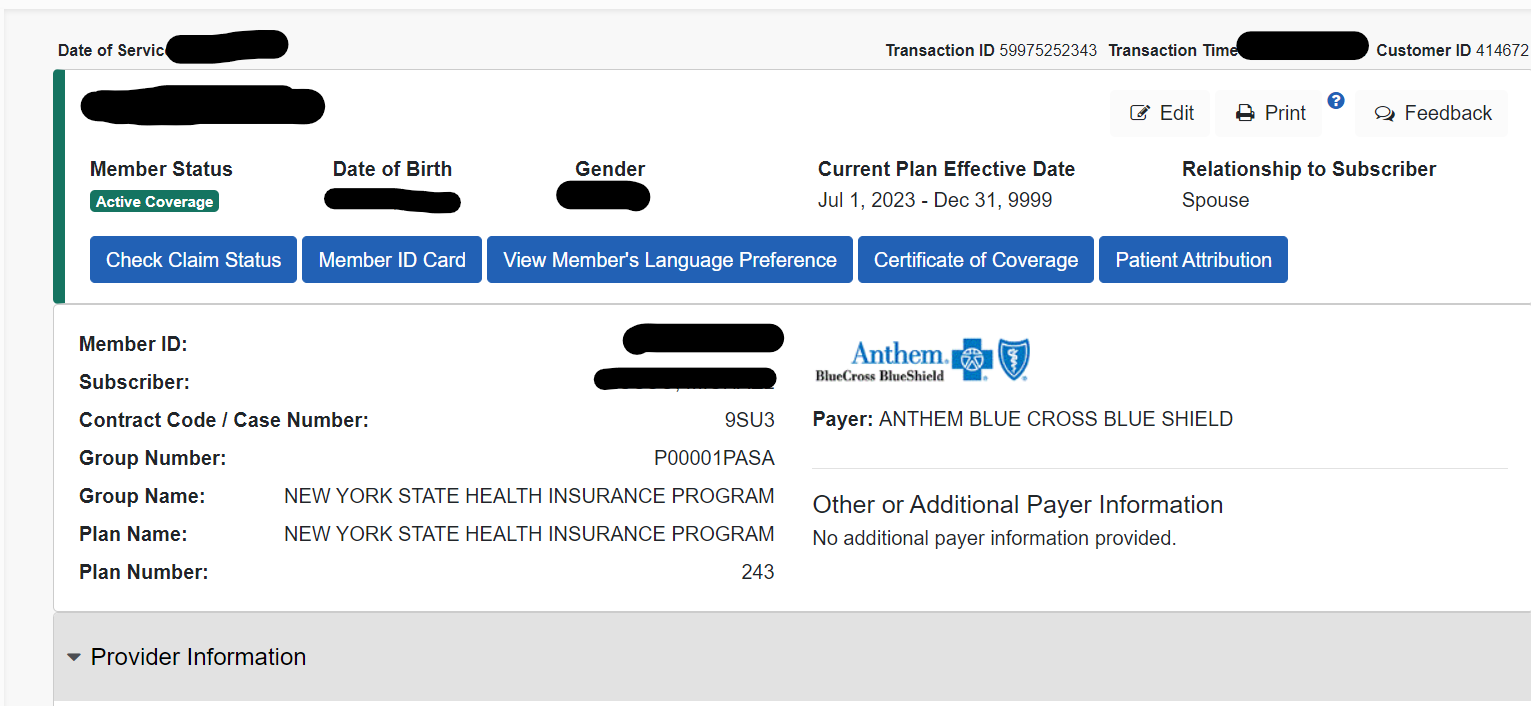
- You can then open the file, we search for the eligibility of a client with his/her Client ID & Date of Birth on the relevant platform (the platform is dependent on the clients’ carrier). Once you put in the details, Click on search and check the ‘Response Text’ – A message stating whether he/she is eligible or ineligible.
- Then input the information on the spreadsheet.
- Once you identify the ineligible Clients, you’d use the format already provided to send the information/report to the appropriate officials/staff.
- Log on to the Smart App
- Click on New Era Rehabilitation Center icon
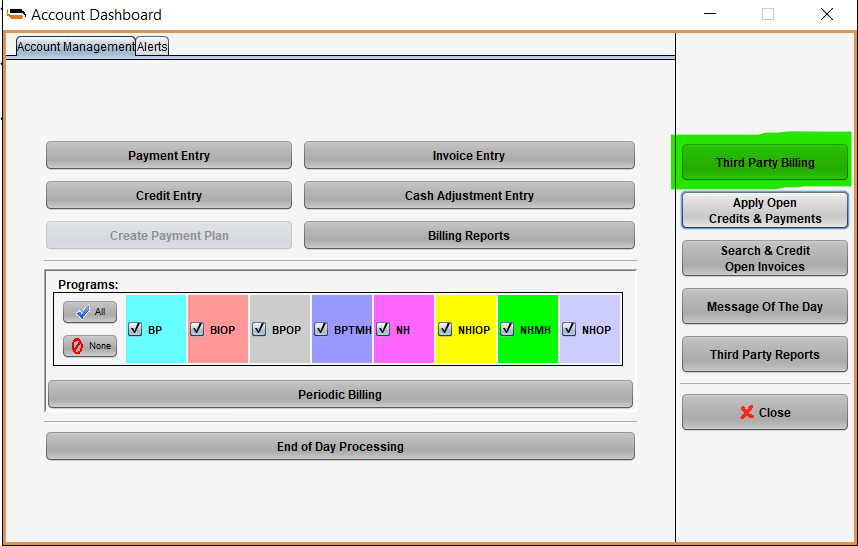
- Click on the dollar sign ---- ‘Third Party Billing’ ---- Eligibility
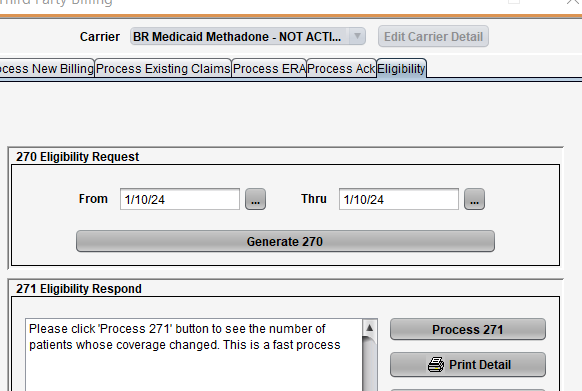
- Ensure the ‘from & thru dates’ reflect the present date. It won’t let you go back
- Don’t change the carrier as long as it is BR Daily Medicaid Methadone – Not Active.
- Click on Generate Report (The file name for Eligibility is 270 & the file we’d receive is called 271)
- You’d see a pop-up that the file has been generated
- Go to New Era EDI on Smart, Click on it, search for Form 270, copy & paste the latest file on your desktop.
- Upload the file on CTDSS, Transaction type - ‘HIPAA (x12 or NCPDP)’
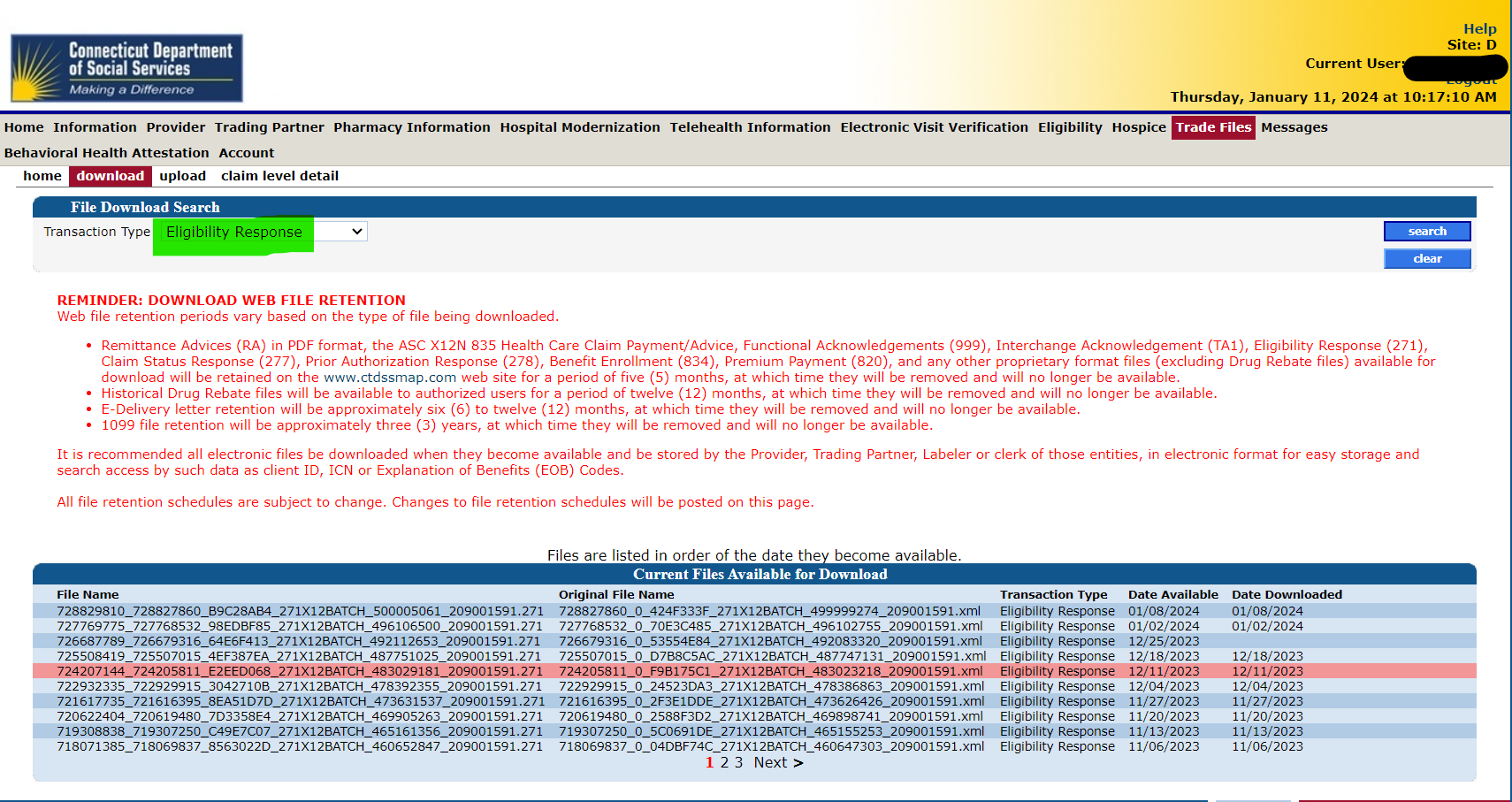
- Within a duration of 15 mins to a day, you’d have a response. To check the response – Go to Trade Files on CTDSS, download, Check ‘Eligibility Response’, download the file & save in EDI.
- Click on Process 271 ---- Go to the file you saved in EDI & click on it. You’d see the document. Save in EDI-OSH – Eligibilty
- Then go through the Eligibility details & identify the clients whose coverage have expired.
- Note them down & send them to the appropriate officials.
** Ensure the run date is correct
** Put in the carrier & program
2nd Way
Note: If you want to check few clients’ eligibility, you’d go to their various insurance sites/availity to check. This differs from our regular prescheduled eligibility check described above.
Have a doubt?
Login