Revenue Cycle Management
Introduction to Revenue Cycle Management
Eligibility
Medical Insurance Authorization
Revenue Reconciliation
Denials
Revenue Recovery
Quiz
Reconciliation 2
HOME HEALTHCARE RECONCILIATION ON UNITED HEALTH PORTAL
- HOW TO GET PROVIDER INFORMATION FOR RECONCILIATION
- Click on the United HealthCare (UTC) Portal to sign in with the assigned user name and password.
- Click on claims and payments
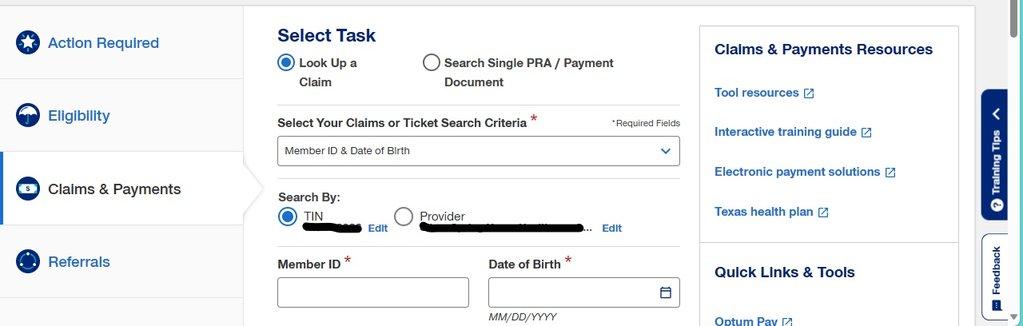
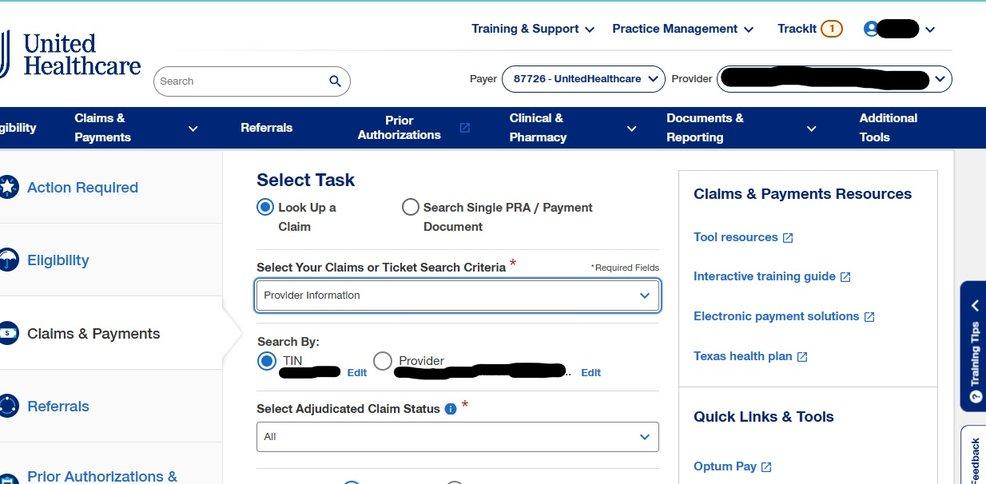
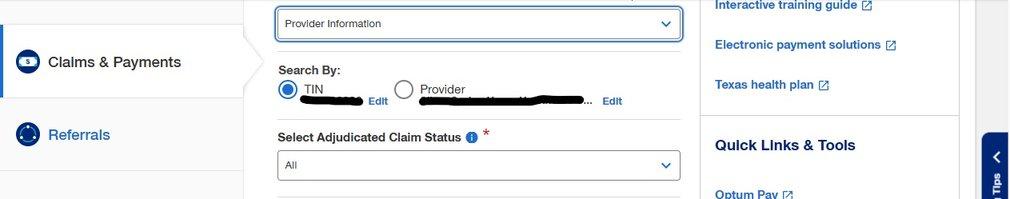
- SELECT YOUR CLAIMS OR TICKET SEARCH CRITERIA has a drop down, click on provider information
- SELECT ADJUDICATED CLAIM STATUS, click ALL
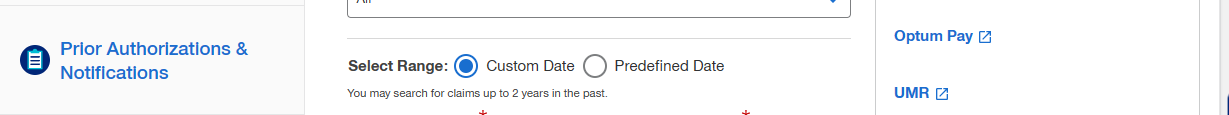
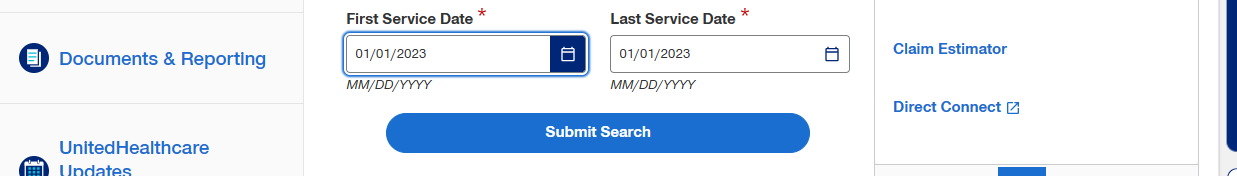
- Select range (custom date)
- Add the range of the service date you’re working with
- Click on Search
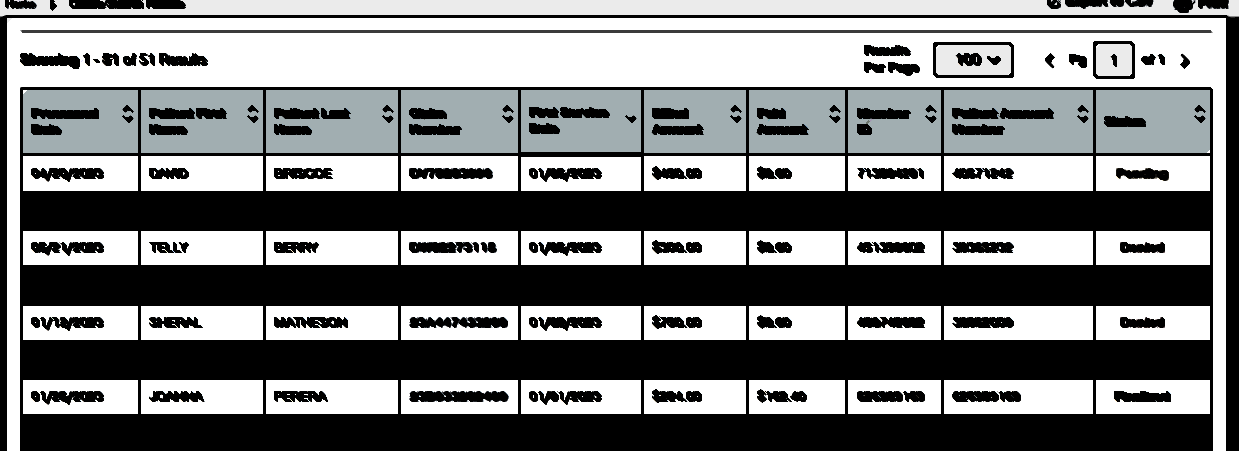
- All information about that range of service date pops up
- Click on Export to CSV (this should be monthly)
- RECONCILAITION
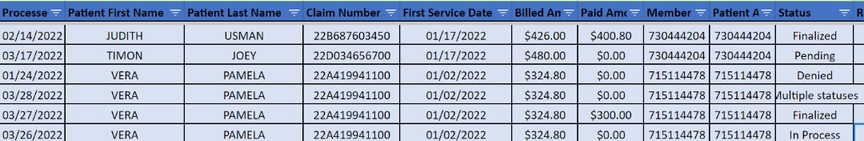
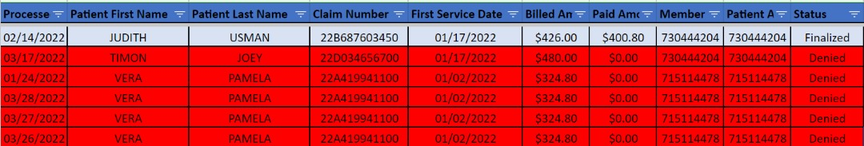
- On the excel sheet you sort by LAST NAME
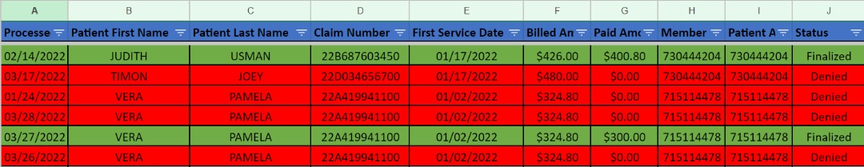
- Create a filter under status which includes Finalized, Denied, Pending, Multiple statuses and In process.
- Colour each of the aforementioned statuses with a preferred colour
- Check for repeated claims that have same clients name, same service dates, same amount and delete but leave the one that has the most recent process date.
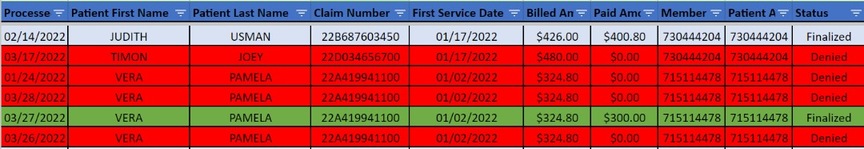
- PLEASE NOTE: In a case where it’s the same clients name, same service dates and same amount but different statuses (FINALIZED or DENIED) please “delete” the denied claim.
- It is advisable to copy all denied claims and paste them on a different sheet because that’s what you will be working with. While on the sheet, create a new column called REASONS
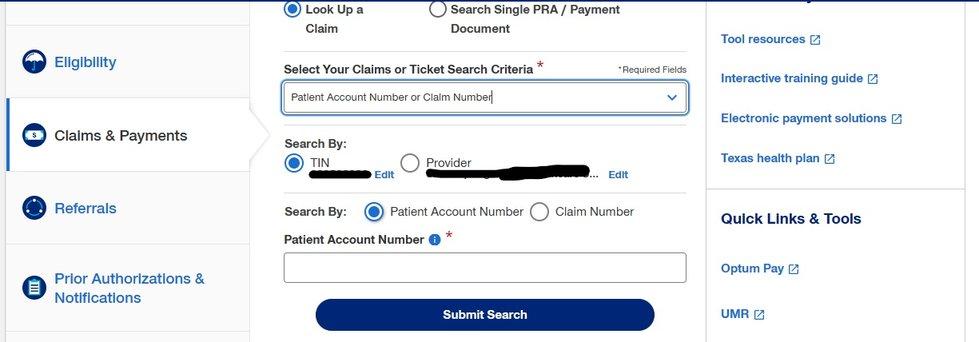
- Copy the Member ID, go to UHC Portal, go to SELECT YOUR CLAIMS OR TICKET SEARCH CRITERIA, select Patient Account Number or Claim Number and submit search.
- Investigate the reasons for denial, copy and paste the reason on the DENIAL SHEET.

Have a doubt?
Login